European countries rushed to buy the antiviral drug in January 2022, but now it’s going to waste. Why?
A COVID-19 antiviral drug has been underused in Europe with about 3.1 million courses of the medicine set to expire in the UK, Germany, Spain, Italy, and France by the end of this month.
Paxlovid emerged as a vital tool against COVID-19, at the beginning of 2022, backed by clinical trial results indicating a nearly 90 per cent reduction in the risk of severe illness.
But the UK-based global health data and analytics company Airfinity said in a report earlier this year that a few of the batches initially delivered by the drug’s manufacturer Pfizer already started expiring in July 2023, according to publicly available data in the five European countries.
It estimates a large number of courses are set to expire between November 2023 and February 2024, which will cost an estimated €2 billion.
Airfinity underlines that this analysis does not include courses available through the European Union supply deal due to a lack of publicly available information about them.
Why is Paxlovid underused in Europe?
European countries rushed to procure the antiviral from Pfizer as soon as the European Medicines Agency (EMA) gave the antiviral drug the green light in January 2022.
The number of infections has since dropped significantly and vaccination rates have reached high levels. With hospitals no longer under pressure due to COVID-19, the need for Paxlovid has decreased, experts say.
"When governments were procuring these treatments, it was essentially the end of 2021, where we had really large spikes in COVID-19 levels. Naturally, they had to prepare for 2022 and 2023 with [anticipated] high COVID-19 levels, and this hasn't necessarily materialised with the worst potential forecast in particular for 2023," Marco Gallotta, Life Science Analyst at Airfinity, told Euronews Health.
The team behind the report said it’s hard to generalise the reasons behind Paxlovid being wasted across Europe, but the criteria for who can receive the drug could be a major factor.
"Naturally, because you are limiting the overall size of the population that can get it," Gallotta said.
"The UK would be a perfect example of this. They've kept these strict prescription criteria throughout the pandemic. Even now, they're among the most limiting, globally," Gallota added.
"This is also the country where we expect the highest wastage".
Other reasons may be how well the treatments have been distributed across the countries and how a prescription is carried out, which may be difficult for healthcare workers.
"Europe could have seen a much higher use of oral antivirals, and we have evidence from other countries where this has actually happened, and they have been able to use much more," said Gallota.
It could depend on its distribution including how far into the pandemic they allowed pharmacies to distribute the drug.
Data from Australia’s health authority Pharmaceutical Benefits Scheme (PBS) suggest that they were prescribing at much higher rates, despite having quite limiting prescription criteria for most of the pandemic, according to Airfinity.
In Australia, Paxlovid is only prescribed to those above a certain age and with risk factors.
"This is not extremely common. Usually age itself, is enough, to receive a prescription for the antivirals, namely those that are either over 60 or 65," said Gallota.
"So even in that situation, they have managed to, reach prescription levels that are much higher than those European countries, which may just, talk more about, their, efficiency, and the efficiency of their scheme, rather than anything else".
France, which started offering Paxlovid in February 2022, simplified access to the drug months later, making it available via prescription after doctors complained about the complex process that resulted in lower-than-expected use.
'Risk balancing is not easy'
The antiviral is often prescribed for patients who have a risk of severe COVID-19 symptoms such as those over the age of 65.
Doctors say difficulties around risk assessment could also be a reason for its underuse.
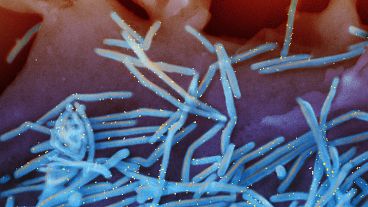
“It consists of two drugs. There's the antiviral drug, the effective one. And then there is another drug, ritonavir, which is an old HIV drug, which boosts the levels of the effective drug,” Asko Järvinen, Head of Infectious Diseases at Helsinki University Hospital (HUS), told Euronews Health.
According to Järvinen, ritonavir also affects the metabolism of many other drugs.
"The risk balancing is not so easy and physicians are not so well informed. It's very tricky for physicians who are not used to evaluating these drug interactions," Järvinen said. This is particularly true for older individuals.
"They usually have many drugs that interact that might be more difficult or more dangerous for them than the COVID disease, at least after vaccinations," Järvinen said.
"Patients have had bleeding or serious drug interactions while they've been on Paxlovid," he added, with some patients also needing to stop medications.
Paxlovid is also only effective when used before the fifth day of COVID-19 symptoms. But it can be hard for the patients to know whether they are at risk and that they need to start the treatments early.
“The problem is that you should start it early on once you get the severe disease, it's not effective anymore. The earlier after you got the infection and the symptoms you started, the more effective it is,” Järvinen said.
Finland saw a similar trend as other European countries, according to the expert, but the drug seems to still help unburden hospitals when infection rates increase.
“If you look at the use in Finland, we used quite a little during 2022 and in early 2023, but during the autumn, when we got the boost of infections, from October onwards, the drug was almost totally sold out in Finland before we got new [doses],” said Järvinen.
He said Finland’s largest healthcare district HUS spent €1 million, compared to around €10 to 20,000 per month in the preceding months.
"We've been trying to educate the people, those who are in the specialised healthcare so that the patients would get the drug from the hospital. So the hospital physician who is in charge of the treatment of the patient would give that," he said.
"Most of the use was when we had most of the infections. And somehow it at least tells you that when the infection burden is high then the drug was used, that the recommendations perhaps worked not on every patient, but in the big picture".
Since the antiviral drug was approved by the European Medicines Agency in January 2022, some 17 EU member states signed bilateral agreements with its manufacturer Pfizer.
The EU secured up to 3.4 million courses of the drug with an additional agreement in November 2022, but it's not clear to which countries they were distributed and how long their shelf lives are.
For more on this story, watch the video in the media player above.